COVID-19, Vitamin D and Saving Lives
Vitamin D is called the ‘sunshine vitamin’ as it is produced in large quantities by the action of sunlight on the skin. The science clearly shows that ‘optimal’ levels of vitamin D (circa 150 nmol/L – UK units) are associated with a significant reduction in the risk of developing a number of chronic diseases (other than osteoporosis) including, but not limited to cancer, diabetes, Alzheimer’s, depression, high blood pressure, autoimmunity, asthma, eczema, multiple sclerosis, cardiovascular disease and respiratory diseases.
There has been a flurry of research/reviews appearing in the literature over the past 6 months discussing/analyzing/questioning the potential role that optimising vitamin D levels might have on reducing the severity of COVID-19. One particular recent preliminary study titled ‘Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study – (Prabowo Raharusuna et al, April 26, 2020) analysed the outcomes of 780 hospitalised COVID-19 patients and concluded that ‘when compared to cases with normal vitamin D status, death was approximately 10.12 times more likely for vitamin D deficient cases’.
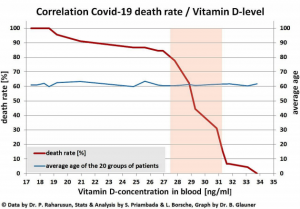
The chart below (taken from the above study) clearly shows that when vitamin D levels are above 32 ng/ml (US measurement) which equates to 80 nmol/L in UK numbers, the risk of death is reduced 10 fold. This very strongly suggests that one of the most effective strategies that you can do, to stay as well as possible, should you ever get COVID-19 is to have optimal levels of vitamin D, which is circa 150 nmol/L.
This is an extraordinary observation that has enormous potential therapeutic and prophylactic implications, especially as supplementing with vitamin D is cheap and easy to do. Another recent review paper titled ‘Point of view: Should COVID-19 patients be supplemented with vitamin D?’ (C Annweiler et al – Maturitas, 2020), analyses the available evidence base according to the ‘Hills Criteria of Causation’ (used to assess evidence of a ‘causal relationship’) and concludes that ‘vitamin D may be considered a biological determinant of COVID-19 outcomes’. This paper then goes on to say that ‘given the lack of specific treatment for COVID-19, the urgency of the pandemic, and the safety of vitamin D supplementation, these observations provide an argument for testing vitamin D as an adjuvant treatment to improve the clinical presentation of COVID-19 and its prognosis’.
A number of randomised controlled trials are now thankfully underway. In the meantime, given the significant evidence base linking ‘optimal’ levels of vitamin D to improved COVID-19 outcomes, why would one not measure current levels (can be done at home using a finger prick test – https://www.revital.co.uk/revital-nhs-vitamin-d-test-kit-kit and https://medichecks.com/products/vitamin-d-25-oh-blood-test are good options) supplement accordingly (a safe dosage to take per day to improve levels would be 5,000 IU) to achieve/maintain optimal levels, especially as there is a great deal of concern about a second wave of COVD-19 in the coming winter? Whilst clearly this will not prevent COVID-19 being contracted, the current data does strongly suggest that it will reduce the risk of potentially fatal complications – thereby protecting the NHS and saving lives.
Please do not simply supplement with vitamin D without testing levels, as it is a fat-soluble vitamin, and can therefore become toxic at high levels. It is also important that you monitor progress (retest every few months) if supplementing with vitamin D, so that the dosage can be adjusted accordingly to achieve/maintain optimal levels. You cannot guess your levels – you have to test. Vitamin D supplementation should always be discussed further with your doctor if you have parathyroid issues, elevated calcium levels, kidney disease or sarcoidosis.
Another key point to consider is that it is generally accepted that Black Asian and Minority Ethnic (BAME) groups living in the West have significantly lower levels of vitamin D compared to their white counterparts. This is due to the fact that the sun is not strong enough to generate sufficient levels of vitamin D due to the sunlight protective effect of increased melanin pigment in the skin. Maybe, just maybe this is one of the most significant reasons as to why a disproportionate number of this group are dying of COVID-19?
It should also be noted that as a nation the UK has one of the highest levels of vitamin D deficiency in Europe, with average levels at 47.4 nmol/L and that it is perfectly possible that this fact is contributing to the high COVID-19 death rate (105 per million) that we are experiencing compared to other countries (on the other end of the scale Slovakia has an average vitamin D level of 81.5 nmol/L and a death rate of 0.4 per million) – ‘The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality’ – Petre Cristian Ilie et al – Aging Clinical and Experimental Research.
So in summary, the evidence base would very strongly suggest that one of the simplest things that you can do to reduce the risk of developing serious complications if you contract COVID-19, is to optimise your vitamin D levels – aiming for circa 150 nmol/L, by testing, supplementing and monitoring your progress.

 RT
RT