Diverticula Disease (Diverticulosis and Diverticulitis) – Extremely Common Yet Poorly Understood
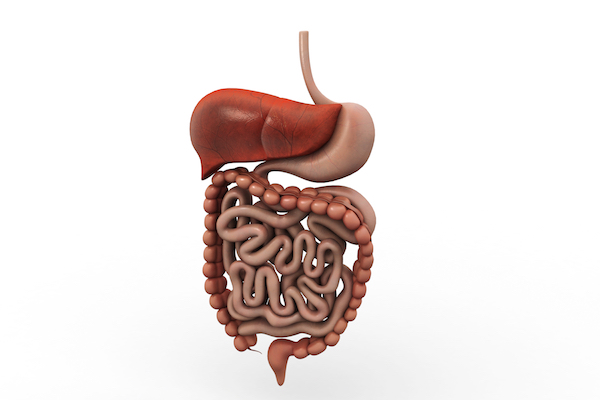
Diverticula disease includes diverticulosis and diverticulitis. Diverticulosis occurs when small pouches or pockets develop in the colon (the large intestine). This is a very common condition occurring in approximately 1 in 3 over the age of 60 and half of 80 year olds. The majority of individuals will have no symptoms with diverticulosis. Diverticulitis is when these pockets become inflamed. This is when symptoms can manifest, with pain in the lower left side of the abdomen being the most common. Other key symptoms include tenderness of the tummy area, cramping, bloating, constipation/diarrhoea, fever, nausea and vomiting. Approximately 25% of individuals with diverticulitis will go onto develop potentially very serious complications including perforations of the gut wall, obstructions and inflammation of the lining of the abdomen. Medical treatments include antibiotics, pain relief and surgery.
Current mainstream dietary advice to help reduce the risks of diverticula disease is based on limited evidence. Advice includes avoiding nuts and seeds and eating more fibre. So what are the key triggers?
Chronic low-grade inflammation and imbalances in the micro ecology of the gut (dysbiosis) are the most significant triggers of diverticula disease. These are of course connected. For those of you that have been reading this column, this will be of no surprise, as the harmonious balance of bacteria in the gut is a fundamental pillar of well-being.
The evidence base and clinical experience suggest that there is a significant correlation between the presence of Small Intestinal Bacterial Overgrowth (SIBO – a type of dysbiosis) and diverticula disease. SIBO is where the small intestine (the part of the digestive system responsible for absorbing nutrients) is overgrown with bacteria that should not be there. This is a notoriously difficult condition to effectively treat, as unless the key factors that caused SIBO to happen in the first place are resolved, then it will typically return no matter whether Rifaxamin (a special non absorbable antibiotic) or antimicrobials are used.
Imbalances that typically trigger the presence of SIBO include poor digestive capacity (weak stomach acid/bile flow and low digestive enzyme status) and poor motility of the small intestine (the migrating motor complex) due to compromised vagus nerve health (often connected to stress). Probiotic and prebiotic supplementation have both been shown to be beneficial, as has shifting diet towards a whole foods anti-inflammatory approach, reducing stress, exercising, undertaking myofascial therapy and using targeted supplementation.

 RT
RT 

Leave a Reply
Want to join the discussion?Feel free to contribute!